
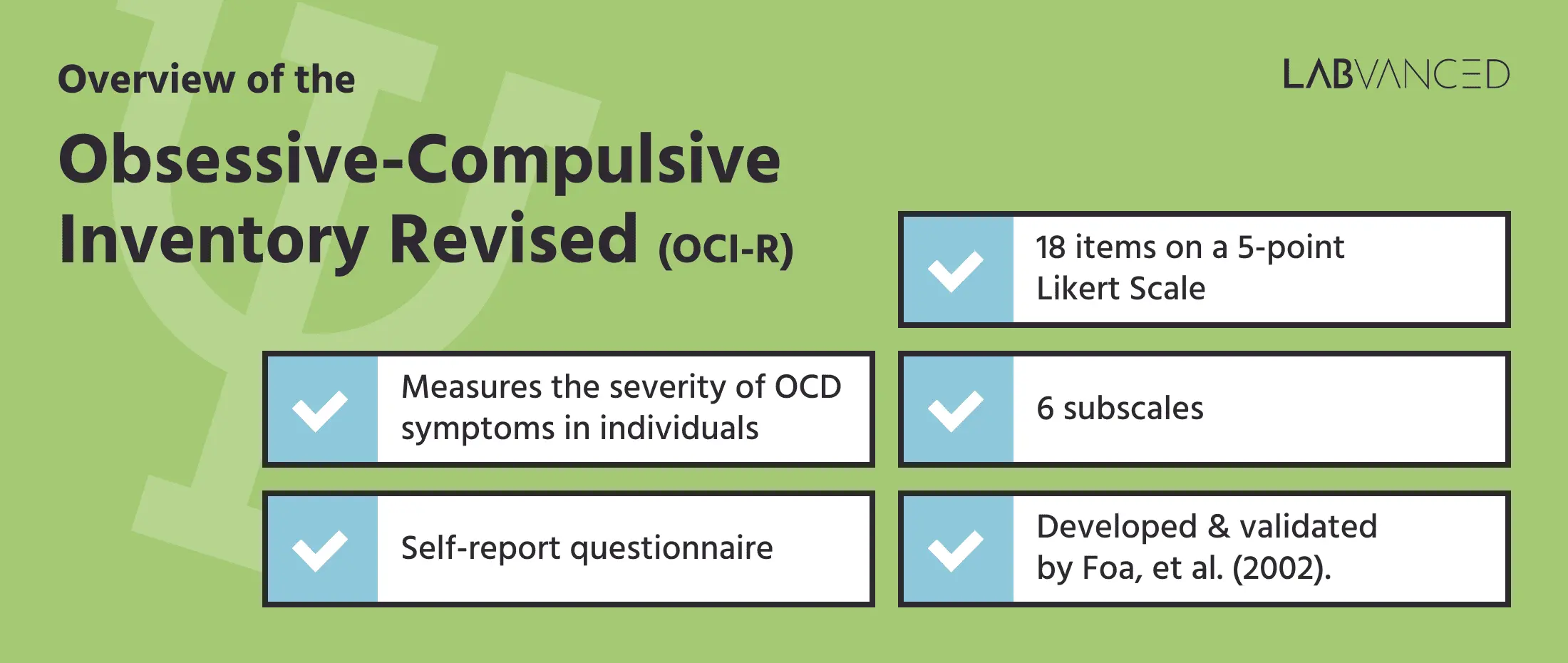
The Obsessive Compulsive Inventory – Revised (OCI-R)
The Obsessive Compulsive Inventory- Revised (OCI-R) is a brief self-report assessment tool used to measure the severity of OCD symptoms in individuals. Obsessive Compulsive Disorder, commonly known as OCD, is a mental health condition in which individuals experience repeated unreasonable thoughts and they engage in rituals (compulsions) in order to manage these thoughts. From being used as a screening tool to determining the severity of OCD, the Obsessive Compulsive Inventory- Revised (OCI-R) has been translated in multiple languages and stands out as a commonly used tool worldwide.
History of the Obsessive Compulsive Inventory – Revised (OCI-R)
The Obsessive Compulsive Inventory- Revised (OCI-R) was first developed by Foa, et al. (2002) as a revised version of the original Obsessive Compulsive Inventory (OCI) developed by Foa and her colleagues in 1998. Despite being psychometrically sound, the 42 items and 7 subscales of the OCI made it lengthy and redundant. To address this issue and to focus on the primary symptoms of OCD, the Obsessive Compulsive Inventory- Revised (OCI-R) was developed (Woo et al., 2010). Several studies tested the psychometric properties of the OCI-R and it was found to have excellent reliability and validity (Abramowitz et al., 2006; Huppert et al., 2007; Koike et al., 2017).
Note: It is important to mention that the OCI-R scale was developed based on the diagnostic framework of DSM-IV when hoarding was still considered to be a part of OCD. However, with the release of DSM-V, hoarding was classified as a separate disorder. Recent studies on the validity of OCI-R based on the DSM-V framework indicated that hoarding subscale is distinct from other subscales of OCI-R (Cervin et al, 2020; Wootton et al, 2015).
Structure of the OCI-R
The OCI-R consists of 18 items rated on a 5-point Likert scale where the choice items are assigned numeric values 0 to 4 based on the severity of symptoms. The respondent is expected to indicate how much, over the past month, the experience described by the questionnaire item distressed or bothered them.
The OCI-R questionnaire, as shown above, can be imported to your Labvanced account and then edited by clicking on the ‘Import’ button here.

These items are further grouped into 6 subscales with 3 items each. The scale is presented with each item distributed in a mixed order so that participants do not get biased by grouping. The scale typically takes 7- 10 minutes to complete (Abramovitch et al., 2020).
Types of Items
Here are a few examples of the questions featured in the OCI-R:
- I have saved up so many things that they get in the way.
- I check things more often than necessary.
- I get upset if objects are not arranged properly.
- I feel compelled to count while I am doing things.
- I find it difficult to touch an object when I know it has been touched by strangers or certain people.
Subscales of the OCI-R
The original OCI had 7 subscales that were created based on the DSM-IV (1994) diagnostic criteria for OCD (Foa et al., 1998). As a development, the OCI-R reduced this number by removing the ‘Doubting’ subscale that it initially included, resulting in the following 6 subscales:
- Washing (items 5, 11, 17): Assesses the difficulty of individuals to touch previously touched objects and has a tendency to repeatedly clean and wash hands due to a sense of contamination.
- Checking (items 2, 8, 14): Assesses the tendency to excessively check items such as doors, windows, etc to prevent any kind or harm or uncertainty.
- Hoarding (items 1,7,13) : Assesses the tendency to collect and store objects that are useless or of little value to others.
- Ordering (items 3, 9, 15): Assesses the tendency to arrange surroundings and objects symmetrically.
- Obsessing (items 6, 12, 18): Assesses the difficulty in controlling unwanted and intrusive thoughts.
- Neutralizing (items 4, 10, 16): Assesses the tendency to engage in mental actions (such as counting numbers) to eliminate the unwanted thoughts.
As mentioned previously, the ‘Hoarding’ subscale is not included in the DSM-V. Time will tell whether a newer version of the OCI-R will be released. For now, researchers are still using this questionnaire in their studies.

Scoring the OCI-R
Based on the participant’s choices, the numeric values assigned to each choice are then added up to acquire a total score. The total score can vary between 0 to 72 (Wootton et al., 2015). For the subscales, the score ranges from 0 to 12. Higher scores indicate greater severity of symptoms. Foa et al. (2002) identified that a score of 21 is the optimal cutoff score for differentiating between individuals with OCD and those without a psychiatric diagnosis, ie. non anxious controls. Furthermore, in a sample with OCD participants and anxious controls, the optimal cut-score for the OCI-R is 18.
The Obsessive Compulsive Inventory – Revised (OCI-R) in Research
The comprehensive and versatile symptom assessment of Obsessive Compulsive Inventory- Revised (OCI-R) makes it a valuable tool in assessing various psychological and behavioral domains. Research on the OCI-R not only provides an understanding of obsessive-compulsive symptoms but also in effectively assessing other disorders that could co-occur with it. Here are a few examples:

Eating Disorders: In the study by Meule and Voderholzer (2022), the OCI-R was utilized to assess obsessive-compulsive symptoms in inpatients with the eating disorder – anorexia nervosa. Patients were required to complete the OCI-R at both admission and discharge. This enabled the researchers to assess the changes in symptom severity over the course of treatment of the participants. The findings showed a significant reduction in OCD symptoms, indicating an association between obsessive-compulsive symptoms and treatment outcomes in anorexia nervosa.
Personality Disorders: The OCI-R was used in a study to understand the correlation between OCD symptoms and specific personality disorders. The participants of the study were individuals diagnosed with OCD. It was found that there was a severity of hoarding and symmetry symptoms in participants with Obsessive-Compulsive Personality Disorder (OCPD), OCD patients with Borderline Personality Disorder (BPD) showed impulsivity and affective instability and with Schizotypal Personality Disorder (SPD) showed higher rates of bipolar disorder, suggesting the increased risk of co-occurring bipolar disorder in OCD patients (Melca et al, 2015).
Anxiety Disorders: In a study by Hassoulas et al. (2021), the authors aimed to assess the relationship between the symptoms assessed by the OCI-R and health-related anxiety. The study was conducted during the COVID-19 pandemic. Of the 332 participants chosen for the study, 254 were found to have significant OCD symptoms. The findings further indicated that individuals with OCD were more likely to experience increased anxiety as related to health and hygiene practices.
Depression & Mood Disorders: The OCI-R was used to assess the presence and severity of OCD symptoms in patients diagnosed with anxiety and depression. It was found that 33% of the sample had major depressive disorder (MDD) and a major 36% of the sample showed symptoms consistent with obsessive-compulsive disorder. The OCI-R proved to be a valuable tool in understanding the complexities of depression and comorbid symptoms of OCD (Orozco et al, 2021).
Post-traumatic stress disorder (PTSD): The Obsessive-Compulsive Inventory–Revised (OCI-R) was utilized in a study to assess the relationship between the severity of OCD symptoms and childhood maltreatment of the participants. The findings indicated that the participants with a history of childhood maltreatment may experience more severe OCD symptoms, particularly individuals with PTSD (Boger et al, 2020).
Conclusion
The Obsessive-Compulsive Inventory-Revised (OCI-R) has proven to be both a versatile and useful tool in understanding the multifaceted nature of Obsessive-Compulsive symptoms. With just 18 items and excellent psychometric properties, it serves as an easy and short test for quantifying OCD-related symptoms that can also be administered across various clinical populations for exploring comorbid conditions like eating disorders, personality disorders, and PTSD. The OCI-R continues to be a valuable resource for clinicians and researchers in enhancing their understanding of OCD pathology and its related complexities!
References
Abramovitch, A., Abramowitz, J. S., Riemann, B. C., & McKay, D. (2020). Severity benchmarks and contemporary clinical norms for the obsessive-compulsive inventory-revised (OCI-R). Journal of Obsessive-Compulsive and Related Disorders, 27, 100557. https://doi.org/10.1016/j.jocrd.2020.100557
Abramowitz, J. S., & Deacon, B. J. (2006). Psychometric Properties and construct validity of the obsessive–compulsive inventory—revised: Replication and extension with a clinical sample. Journal of Anxiety Disorders, 20(8), 1016–1035. https://doi.org/10.1016/j.janxdis.2006.03.001
Boger, S., Ehring, T., Schwarzkopf, W., & Werner, G. G. (2020). Potential mediators of the association between childhood maltreatment and obsessive-compulsive disorder in adulthood. Journal of Obsessive-Compulsive and Related Disorders, 27, 100587. https://doi.org/10.1016/j.jocrd.2020.100587
Cervin, M., Perrin, S., Olsson, E., Aspvall, K., Geller, D. A., Wilhelm, S., McGuire, J., Lázaro, L., Martínez-González, A. E., Barcaccia, B., Pozza, A., Goodman, W. K., Murphy, T. K., Seçer, İ., Piqueras, J. A., Rodríguez-Jiménez, T., Godoy, A., Rosa-Alcázar, A. I., Rosa-Alcázar, Á., … Mataix-Cols, D. (2020). The centrality of doubting and checking in the network structure of obsessive-compulsive symptom dimensions in youth. Journal of the American Academy of Child & Adolescent Psychiatry, 59(7), 880–889. https://doi.org/10.1016/j.jaac.2019.06.018
Foa, E. B., Huppert, J. D., Leiberg, S., Langner, R., Kichic, R., Hajcak, G., & Salkovskis, P. M. (2002). The obsessive-compulsive inventory: Development and validation of a short version. Psychological Assessment, 14(4), 485–496. https://doi.org/10.1037/1040-3590.14.4.485
Foa, E. B., Kozak, M. J., Salkovskis, P. M., Coles, M. E., & Amir, N. (1998). The validation of a new obsessive–compulsive disorder scale: The Obsessive–Compulsive Inventory. Psychological assessment, 10(3), 206.
Hassoulas, A., Umla-Runge, K., Zahid, A., Adams, O., Green, M., Hassoulas, A., & Panayiotou, E. (2021). Investigating the association between obsessive-compulsive disorder symptom subtypes and health anxiety as impacted by the COVID-19 pandemic: A cross-sectional study. Psychological Reports, 125(6), 3006–3027. https://doi.org/10.1177/00332941211040437
Huppert, J. D., Walther, M. R., Hajcak, G., Yadin, E., Foa, E. B., Simpson, H. B., & Liebowitz, M. R. (2007). The OCI-R: Validation of the subscales in a clinical sample. Journal of Anxiety Disorders, 21(3), 394–406. https://doi.org/10.1016/j.janxdis.2006.05.006
Koike, H., Tsuchiyagaito, A., Hirano, Y., Oshima, F., Asano, K., Sugiura, Y., Kobori, O., Ishikawa, R., Nishinaka, H., Shimizu, E., & Nakagawa, A. (2017). Reliability and validity of the Japanese version of the obsessive-compulsive inventory-revised (OCI-R). Current Psychology, 39(1), 89–95. https://doi.org/10.1007/s12144-017-9741-2
Melca, I. A., Yücel, M., Mendlowicz, M. V., de Oliveira-Souza, R., & Fontenelle, L. F. (2015). The correlates of obsessive–compulsive, schizotypal, and borderline personality disorders in obsessive–compulsive disorder. Journal of Anxiety Disorders, 33, 15–24. https://doi.org/10.1016/j.janxdis.2015.04.004
Meule, A., & Voderholzer, U. (2022). Changes in obsessive–compulsive symptoms during inpatient treatment of anorexia nervosa. Journal of Eating Disorders, 10(1). https://doi.org/10.1186/s40337-022-00629-3
Orozco, A., Cardoner, N., Aragón, C. F., Ruiz-Murugarren, S., Vicens, M., Álvarez-Mon, M. Á., & Lahera, G. (2021). Obsessive–compulsive symptoms in anxiety and depressive disorders: Influence of recent and/or traumatic life events. Revista de Psiquiatría y Salud Mental, 14(4), 218–226. https://doi.org/10.1016/j.rpsm.2020.12.002
Woo, C.-W., Kwon, S.-M., Lim, Y.-J., & Shin, M.-S. (2010). The obsessive-compulsive inventory-revised (OCI-R): Psychometric properties of the Korean version and the order, gender, and cultural effects. Journal of Behavior Therapy and Experimental Psychiatry, 41(3), 220–227. https://doi.org/10.1016/j.jbtep.2010.01.006
Wootton, B. M., Diefenbach, G. J., Bragdon, L. B., Steketee, G., Frost, R. O., & Tolin, D. F. (2015). A contemporary psychometric evaluation of the Obsessive Compulsive Inventory—revised (OCI-R). Psychological Assessment, 27(3), 874–882. https://doi.org/10.1037/pas0000075